IVF - Fertilization in vitro

IVF - Fertilization in vitro
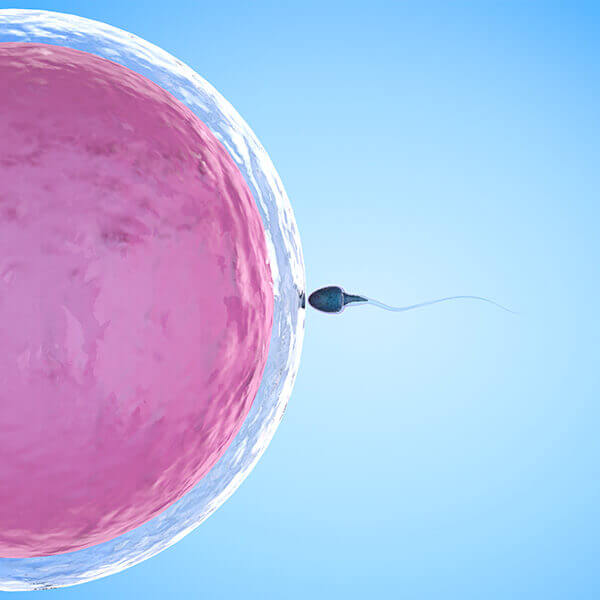
IVF is a process during which an egg is fertilized by sperm outside the woman’s body (in vitro). It is one of the main methods of assisted reproduction used to treat infertility.
This method involves hormonal stimulation of the ovaries to produce more follicles on the surface of the ovary from which a greater number of eggs can be retrieved.
Stimulation is monitored by ultrasound. When the follicles reach the desired size, the stage of preparation for egg retrieval occurs – OPU. The patient is given an injection of hCG hormone (36 to 40 hours before egg collection).
A partner must be present on the day of OPU to provide a sperm sample (unless the couple chooses to use frozen or donated sperm). After the OPU, the couple is informed about the quantity and quality of the eggs and the embryologist chooses the appropriate laboratory methods (ICSI, PICSI, AH, Embryoscope, EmbryoGlue, IMSI, EC…) taking into account the client’s wishes.
OPU – ovum pick up
The eggs are collected under general anesthesia and the procedure takes 15 to 30 minutes. After OPU, the patient is transferred to the recovery room, where she rests for 2 hours and then can go home with her companion.
The male partner must be present on the day of the OPU to provide a sperm sample. After OPU, the couple is informed about the quantity and quality of the eggs and the embryologist chooses the use of special laboratory methods (ICSI, PICSI, AH, Embryoscope, EmbryoGlue, IMSI, EC…)